
What to expect:

Obesity is a chronic disease that causes pathologic changes associated with cardiovascular disease (CVD).1 Excess and dysfunctional adipose tissue is a driver of inflammation and other subclinical CVD markers;2,3 processes that are underway before the metabolic disorders become apparent, indicating that for many patients with overweight and obesity the development of metabolic abnormalities and CVD is just a matter of time.4,5
Obesity has both direct and indirect effects on the development of cardiovascular disease (CVD): it contributes directly to the development of CVD risk factors including hypertension, dyslipidaemia, insulin resistance and diabetes.6,7 But as a chronic and progressive disease itself, obesity has now been shown to be a risk factor for CVD independently of other metabolic abnormalities. 1,4,8,9
People with no metabolic risk factors such as hypertension, dyslipidaemia or diabetes, and who are otherwise healthy but who have overweight or obesity, are nonetheless at increased risk of CVD simply because of their excess weight.4,8
High body mass index (BMI) has now overtaken smoking in the rankings of modifiable risk factors for cardiovascular disease (CVD).6
Obesity is an important modifiable risk factor which can be addressed at the primary care level to help patients reduce their CVD risk, change the course of disease and also improve their outcomes in diabetes, hypertension and dyslipidaemia.10,11
To read more about the complications associated with obesity, click here.
A recent large population study has shown that any level of excess weight is associated with a steep increase in the risk of heart attack, stroke and heart failure as rising BMI compounds the overall CVD risk.8
The study, of approximately 3.5 million individuals who accrued 165,302 CVD events during a 5.4-year average follow-up, showed that individuals who have obesity and are classified as metabolically healthy are still at an increased risk for coronary heart disease, cerebrovascular disease, and heart failure compared with individuals who are normal weight with no metabolic risk factors, underscoring the need for physicians to intervene early and appropriately on obesity.8
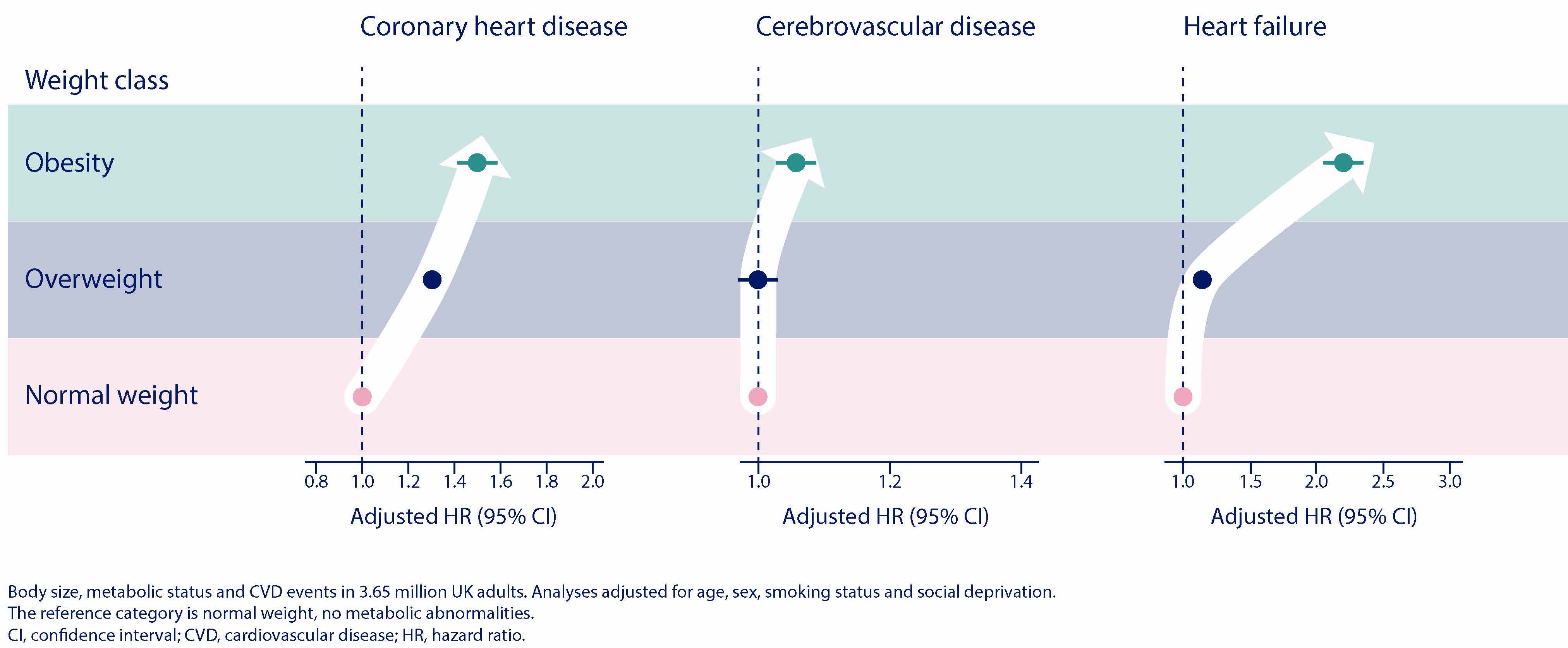 This research has challenged the
concept of metabolically healthy obesity, where an individual can have
a high BMI that is not associated with any metabolic disorder by
demonstrating that people with obesity remain at increased risk of
cardiovascular disease even without metabolic abnormalities5,8
This research has challenged the
concept of metabolically healthy obesity, where an individual can have
a high BMI that is not associated with any metabolic disorder by
demonstrating that people with obesity remain at increased risk of
cardiovascular disease even without metabolic abnormalities5,8
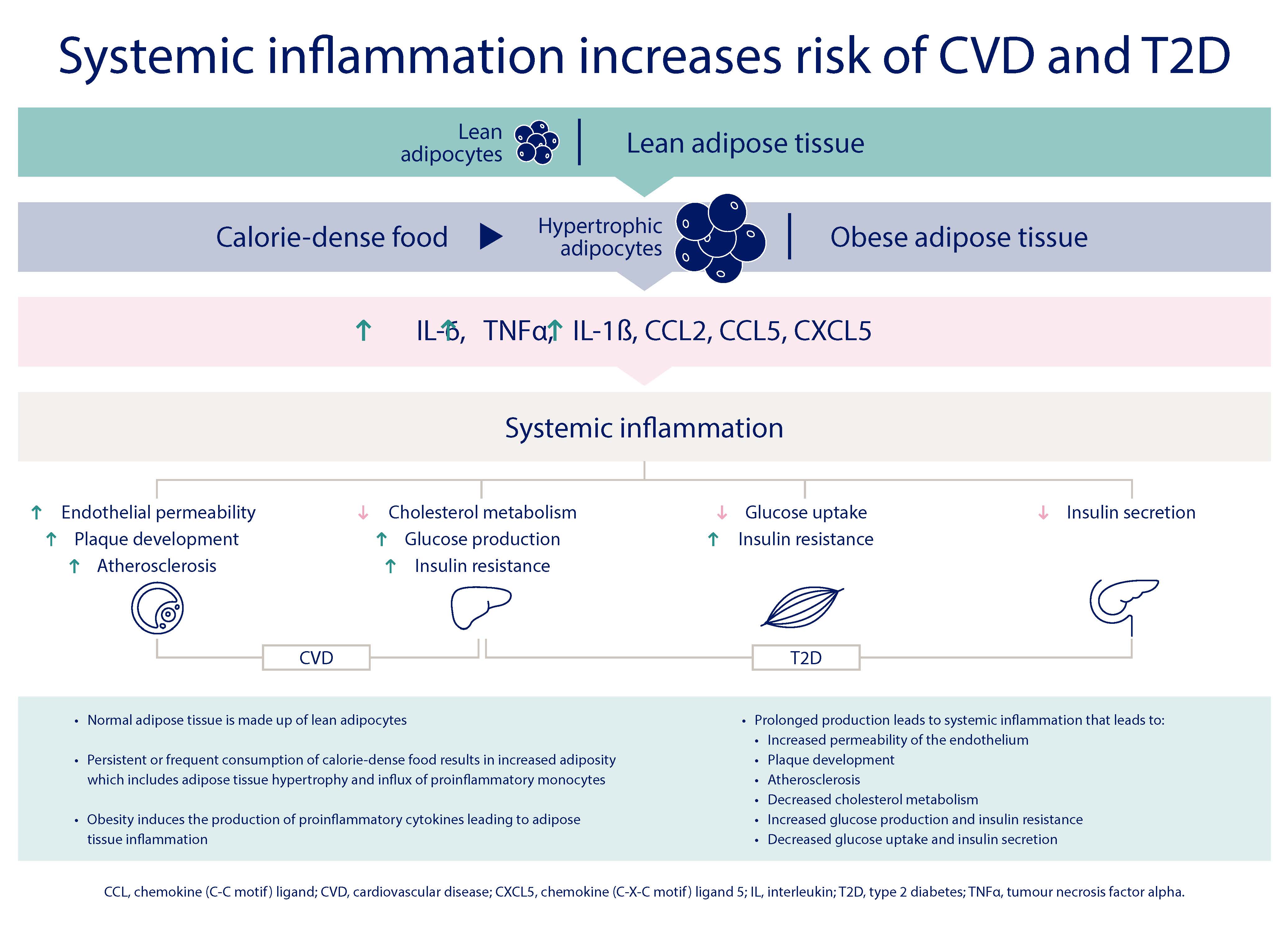
Obesity alters the functioning of adipose tissue so that patients with obesity experience degeneration of their inflammatory markers resulting in systemic inflammation.2,3 Excess weight in the form of fat causes systemic inflammation through the release of proinflammatory cytokines and chemokines produced by the dysfunctional adipose tissue.2 Systemic inflammation reduces insulin secretion and glucose uptake resulting in insulin resistance. It also interferes with cholesterol metabolism and leads to plaque developing in the arteries, resulting in atherosclerosis and increased risk of CVD.2
Additionally, not all excess weight is equal. It has been shown that a relatively larger waist circumference, denoting greater abdominal adipose tissue, or visceral adiposity, is itself a further independent risk factor for CVD.4,12 Indeed, the prospective study, of more than 7,000 people, found that a higher waist circumference was associated with a higher risk of CVD at all levels of BMI, including for people in the normal weight category.4
Additionally, not all excess weight is equal. It has been shown that
a relatively larger waist circumference, denoting greater abdominal
adipose tissue, or visceral adiposity, is itself a further independent
risk factor for CVD.4,12 Indeed, the prospective study, of
more than 7,000 people, found that a higher waist circumference was
associated with a higher risk of CVD at all levels of BMI, including
for people in the normal weight category.4
Systemic inflammation plays an important role in the development of cardiovascular disease, explaining why even when patients’ metabolic abnormalities are being optimally controlled with medications, there remains residual cardiovascular risk to patients from excess weight itself.13
It has been shown that even when patients with overweight or obesity are receiving pharmacologic treatments for their CVD risk factors, they continue to have higher levels of subclinical CVD markers than people without overweight or obesity, including more coronary artery calcium, greater left ventricular mass and greater thickening of the walls of the carotid artery.7
In spite of being treated with up-to-date, evidence-based therapies for hypertension, dyslipidaemia, diabetes and atrial fibrillation, patients with overweight or obesity retain the residual added risk of coronary death or non-fatal myocardial infarction, or fatal or non-fatal stroke.2,3,14
Weight loss is associated with reduced adipose and systemic inflammation and can help patients reduce this residual cardiovascular risk.13
For more information on obesity and CVD morbidity and mortality, click here.
HQ22OB00141, Approval date: October 2022
The site you are entering is not the property of, nor managed by, Novo Nordisk. Novo Nordisk assumes no responsibility for the content of sites not managed by Novo Nordisk. Furthermore, Novo Nordisk is not responsible for, nor does it have control over, the privacy policies of these sites.
At Novo Nordisk we want to provide Healthcare Professionals (HCPs) with scientific information, resources and tools.